Guillain-Barré syndrome can affect
anybody. It can strike at any age and both sexes are equally prone to
the disorder. The
syndrome is rare, however,
afflicting only about one person in 100,000. Usually Guillain-Barré
occurs a few days or weeks
after the patient has had symptoms
of a respiratory or gastrointestinal viral infection. Occasionally
surgery will trigger
the syndrome. In rare instances
vaccinations may increase the risk of GBS.
After the first clinical manifestations of the disease, the symptoms can progress over the course of hours, days, or weeks. Most people reach the stage of greatest weakness within the first 2 weeks after symptoms appear, and by the third week of the illness 90 percent of all patients are at their weakest.
After the first clinical manifestations of the disease, the symptoms can progress over the course of hours, days, or weeks. Most people reach the stage of greatest weakness within the first 2 weeks after symptoms appear, and by the third week of the illness 90 percent of all patients are at their weakest.
What causes Guillain-Barré syndrome?
No one yet knows why Guillain-Barré — which is not contagious — strikes some people and not others. Nor does anyone know exactly
what sets the disease in motion.
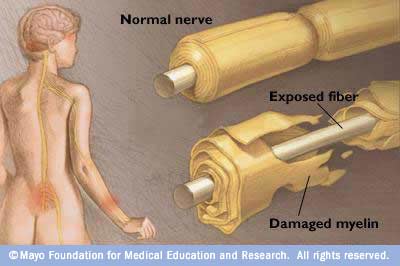
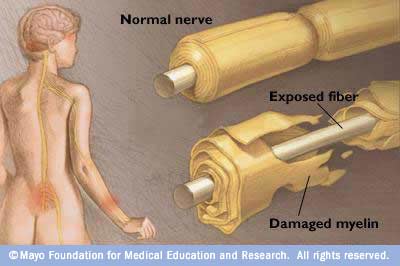
What scientists do know is that the body's immune system begins to attack the body itself, causing what is known as an autoimmune disease. Usually the cells of the immune system attack only foreign material and invading organisms. In Guillain-Barré syndrome, however, the immune system starts to destroy the myelin sheath that surrounds the axons of many peripheral nerves, or even the axons themselves (axons are long, thin extensions of the nerve cells; they carry nerve signals). The myelin sheath surrounding the axon speeds up the transmission of nerve signals and allows the transmission of signals over long distances.
In diseases in which the peripheral nerves' myelin sheaths are injured or degraded, the nerves cannot transmit signals efficiently. That is why the muscles begin to lose their ability to respond to the brain's commands, commands that must be carried through the nerve network. The brain also receives fewer sensory signals from the rest of the body, resulting in an inability to feel textures, heat, pain, and other sensations. Alternately, the brain may receive inappropriate signals that result in tingling, "crawling-skin," or painful sensations. Because the signals to and from the arms and legs must travel the longest distances they are most vulnerable to interruption. Therefore, muscle weakness and tingling sensations usually first appear in the hands and feet and progress upwards.

When Guillain-Barré is preceded by a viral or bacterial infection, it is possible that the virus has changed the nature of cells in the nervous system so that the immune system treats them as foreign cells. It is also possible that the virus makes the immune system itself less discriminating about what cells it recognizes as its own, allowing some of the immune cells, such as certain kinds of lymphocytes and macrophages, to attack the myelin. Sensitized T lymphocytes cooperate with B lymphocytes to produce antibodies against components of the myelin sheath and may contribute to destruction of the myelin. In two forms of GBS, axons are attacked by antibodies against the bacteria Campylobacter jejuni, which react with proteins of the peripheral nerves. Acute motor axonal neuropathy is particularly common in Chinese children. Scientists are investigating these and other possibilities to find why the immune system goes awry in Guillain-Barré syndrome and other autoimmune diseases. The cause and course of Guillain-Barré syndrome is an active area of neurological investigation, incorporating the cooperative efforts of neurological scientists, immunologists, and virologists.
What scientists do know is that the body's immune system begins to attack the body itself, causing what is known as an autoimmune disease. Usually the cells of the immune system attack only foreign material and invading organisms. In Guillain-Barré syndrome, however, the immune system starts to destroy the myelin sheath that surrounds the axons of many peripheral nerves, or even the axons themselves (axons are long, thin extensions of the nerve cells; they carry nerve signals). The myelin sheath surrounding the axon speeds up the transmission of nerve signals and allows the transmission of signals over long distances.
In diseases in which the peripheral nerves' myelin sheaths are injured or degraded, the nerves cannot transmit signals efficiently. That is why the muscles begin to lose their ability to respond to the brain's commands, commands that must be carried through the nerve network. The brain also receives fewer sensory signals from the rest of the body, resulting in an inability to feel textures, heat, pain, and other sensations. Alternately, the brain may receive inappropriate signals that result in tingling, "crawling-skin," or painful sensations. Because the signals to and from the arms and legs must travel the longest distances they are most vulnerable to interruption. Therefore, muscle weakness and tingling sensations usually first appear in the hands and feet and progress upwards.

When Guillain-Barré is preceded by a viral or bacterial infection, it is possible that the virus has changed the nature of cells in the nervous system so that the immune system treats them as foreign cells. It is also possible that the virus makes the immune system itself less discriminating about what cells it recognizes as its own, allowing some of the immune cells, such as certain kinds of lymphocytes and macrophages, to attack the myelin. Sensitized T lymphocytes cooperate with B lymphocytes to produce antibodies against components of the myelin sheath and may contribute to destruction of the myelin. In two forms of GBS, axons are attacked by antibodies against the bacteria Campylobacter jejuni, which react with proteins of the peripheral nerves. Acute motor axonal neuropathy is particularly common in Chinese children. Scientists are investigating these and other possibilities to find why the immune system goes awry in Guillain-Barré syndrome and other autoimmune diseases. The cause and course of Guillain-Barré syndrome is an active area of neurological investigation, incorporating the cooperative efforts of neurological scientists, immunologists, and virologists.
How is Guillain-Barré syndrome diagnosed?
Guillain-Barré is called a syndrome
rather than a disease because it is not clear that a specific
disease-causing agent is
involved. A syndrome is a medical
condition characterized by a collection of symptoms (what the patient
feels) and signs (what
a doctor can observe or measure).
The signs and symptoms of the syndrome can be quite varied, so doctors
may, on rare occasions,
find it difficult to diagnose
Guillain-Barré in its earliest stages.
Several disorders have symptoms similar to those found in Guillain-Barré, so doctors examine and question patients carefully before making a diagnosis. Collectively, the signs and symptoms form a certain pattern that helps doctors differentiate Guillain-Barré from other disorders. For example, physicians will note whether the symptoms appear on both sides of the body (most common in Guillain-Barré) and the quickness with which the symptoms appear (in other disorders, muscle weakness may progress over months rather than days or weeks). In Guillain-Barré, reflexes such as knee jerks are usually lost. Because the signals traveling along the nerve are slower, a nerve conduction velocity (NCV) test can give a doctor clues to aid the diagnosis. In Guillain-Barré patients, the cerebrospinal fluid that bathes the spinal cord and brain contains more protein than usual. Therefore a physician may decide to perform a spinal tap, a procedure in which a needle is inserted into the patient's lower back and a small amount of cerebrospinal fluid from the spinal column is withdrawn for study..

Several disorders have symptoms similar to those found in Guillain-Barré, so doctors examine and question patients carefully before making a diagnosis. Collectively, the signs and symptoms form a certain pattern that helps doctors differentiate Guillain-Barré from other disorders. For example, physicians will note whether the symptoms appear on both sides of the body (most common in Guillain-Barré) and the quickness with which the symptoms appear (in other disorders, muscle weakness may progress over months rather than days or weeks). In Guillain-Barré, reflexes such as knee jerks are usually lost. Because the signals traveling along the nerve are slower, a nerve conduction velocity (NCV) test can give a doctor clues to aid the diagnosis. In Guillain-Barré patients, the cerebrospinal fluid that bathes the spinal cord and brain contains more protein than usual. Therefore a physician may decide to perform a spinal tap, a procedure in which a needle is inserted into the patient's lower back and a small amount of cerebrospinal fluid from the spinal column is withdrawn for study..

How is Guillain-Barré treated?
There is no known cure for
Guillain-Barré syndrome. However, there are therapies that lessen the
severity of the illness and
accelerate the recovery in most
patients. There are also a number of ways to treat the complications of
the disease.
Currently, plasma exchange (also called plasmapheresis) and high-dose immunoglobulin therapy are used. Both of them are equally effective, but immunoglobulin is easier to administer. Plasma exchange is a method by which whole blood is removed from the body and processed so that the red and white blood cells are separated from the plasma, or liquid portion of the blood. The blood cells are then returned to the patient without the plasma, which the body quickly replaces. Scientists still don't know exactly why plasma exchange works, but the technique seems to reduce the severity and duration of the Guillain-Barré episode. This may be because plasmapheresis can remove antibodies and other immune cell-derived factors that could contribute to nerve damage.
In high-dose immunoglobulin therapy, doctors give intravenous injections of the proteins that, in small quantities, the immune system uses naturally to attack invading organisms. Investigators have found that giving high doses of these immunoglobulins, derived from a pool of thousands of normal donors, to Guillain-Barré patients can lessen the immune attack on the nervous system. Investigators don't know why or how this works, although several hypotheses have been proposed.
The use of steroid hormones has also been tried as a way to reduce the severity of Guillain-Barré, but controlled clinical trials have demonstrated that this treatment not only is not effective but may even have a deleterious effect on the disease.
The most critical part of the treatment for this syndrome consists of keeping the patient's body functioning during recovery of the nervous system. This can sometimes require placing the patient on mechanical ventilatory assistance, a heart monitor, or other machines that assist body function. The need for this sophisticated machinery is one reason why Guillain-Barré syndrome patients are usually treated in hospitals, often in an intensive care ward. In the hospital, doctors can also look for and treat the many problems that can afflict any paralyzed patient - complications such as pneumonia or bed sores.
Often, even before recovery begins, caregivers may be instructed to manually move the patient's limbs to help keep the muscles flexible and strong and to prevent venous sludging (the buildup of red blood cells in veins, which could lead to reduced blood flow) in the limbs which could result in deep vein thrombosis. Later, as the patient begins to recover limb control, physical therapy begins. Carefully planned clinical trials of new and experimental therapies are the key to improving the treatment of patients with Guillain-Barré syndrome. Such clinical trials begin with the research of basic and clinical scientists who, working with clinicians, identify new approaches to treating patients with the disease.
Currently, plasma exchange (also called plasmapheresis) and high-dose immunoglobulin therapy are used. Both of them are equally effective, but immunoglobulin is easier to administer. Plasma exchange is a method by which whole blood is removed from the body and processed so that the red and white blood cells are separated from the plasma, or liquid portion of the blood. The blood cells are then returned to the patient without the plasma, which the body quickly replaces. Scientists still don't know exactly why plasma exchange works, but the technique seems to reduce the severity and duration of the Guillain-Barré episode. This may be because plasmapheresis can remove antibodies and other immune cell-derived factors that could contribute to nerve damage.
In high-dose immunoglobulin therapy, doctors give intravenous injections of the proteins that, in small quantities, the immune system uses naturally to attack invading organisms. Investigators have found that giving high doses of these immunoglobulins, derived from a pool of thousands of normal donors, to Guillain-Barré patients can lessen the immune attack on the nervous system. Investigators don't know why or how this works, although several hypotheses have been proposed.
The use of steroid hormones has also been tried as a way to reduce the severity of Guillain-Barré, but controlled clinical trials have demonstrated that this treatment not only is not effective but may even have a deleterious effect on the disease.
The most critical part of the treatment for this syndrome consists of keeping the patient's body functioning during recovery of the nervous system. This can sometimes require placing the patient on mechanical ventilatory assistance, a heart monitor, or other machines that assist body function. The need for this sophisticated machinery is one reason why Guillain-Barré syndrome patients are usually treated in hospitals, often in an intensive care ward. In the hospital, doctors can also look for and treat the many problems that can afflict any paralyzed patient - complications such as pneumonia or bed sores.
Often, even before recovery begins, caregivers may be instructed to manually move the patient's limbs to help keep the muscles flexible and strong and to prevent venous sludging (the buildup of red blood cells in veins, which could lead to reduced blood flow) in the limbs which could result in deep vein thrombosis. Later, as the patient begins to recover limb control, physical therapy begins. Carefully planned clinical trials of new and experimental therapies are the key to improving the treatment of patients with Guillain-Barré syndrome. Such clinical trials begin with the research of basic and clinical scientists who, working with clinicians, identify new approaches to treating patients with the disease.
What is the long-term outlook for those with Guillain-Barré syndrome?
Guillain-Barré syndrome can be a
devastating disorder because of its sudden and unexpected onset. In
addition, recovery is
not necessarily quick. As noted
above, patients usually reach the point of greatest weakness or
paralysis days or weeks after
the first symptoms occur. Symptoms
then stabilize at this level for a period of days, weeks, or, sometimes,
months. The recovery
period may be as little as a few
weeks or as long as a few years. About 30 percent of those with
Guillain-Barré still have
a residual weakness after 3 years.
About 3 percent may suffer a relapse of muscle weakness and tingling
sensations many years
after the initial attack.
Guillain-Barré syndrome patients face not only physical difficulties, but emotionally painful periods as well. It is often extremely difficult for patients to adjust to sudden paralysis and dependence on others for help with routine daily activities. Patients sometimes need psychological counseling to help them adapt.

Guillain-Barré syndrome patients face not only physical difficulties, but emotionally painful periods as well. It is often extremely difficult for patients to adjust to sudden paralysis and dependence on others for help with routine daily activities. Patients sometimes need psychological counseling to help them adapt.

What research is being done?
Scientists are concentrating on
finding new treatments and refining existing ones. Scientists are also
looking at the workings
of the immune system to find which
cells are responsible for beginning and carrying out the attack on the
nervous system.
The fact that so many cases of
Guillain-Barré begin after a viral or bacterial infection suggests that
certain characteristics
of some viruses and bacteria may
activate the immune system inappropriately. Investigators are searching
for those characteristics.
Certain proteins or peptides in
viruses and bacteria may be the same as those found in myelin, and the
generation of antibodies
to neutralize the invading viruses
or bacteria could trigger the attack on the myelin sheath. As noted
previously, neurological
scientists, immunologists,
virologists, and pharmacologists are all working collaboratively to
learn how to prevent this disorder
and to make better therapies
available when it strikes.
 |

